This procedure is designed to relieve arm pain and or numbness and weakness affecting the arms or the legs due to pressure on the spinal cord and or nerve roots. This operation is not designed to relieve neck pain.
Once you are anaesthetised, you are placed face up on the operating table. A horizontal, gently curved incision, approximately 3 cm long, is made just to the right of the Adam’s apple usually within an existing skin crease. We use an X-ray machine (Image Intensifier) to help us locate the correct position. Local anaesthetic is used to numb the nerves in this area and so lighten the anaesthetic needed. The muscles on the side of the neck are then parted and a path taken to the front of the spine. The correct level is then again confirmed with an X-ray. Special retractors are used to hold the soft tissues safely aside – these include the larynx (wind pipe), the oesophagus (swallowing tube), carotid artery and jugular vein. Another special distractor instrument is then used to hold the vertebral bones slightly apart so as to create space to work in. It spans the bones and discs to be operated on/removed. The operating microscope is then brought in and the surgeon operates thereafter looking through this – it brings superb illumination as well as magnification to allow precise operating. Everything up to this point is referred to as “access”. Now the operation proper begins.
The front part of the discs and bones are cleared.
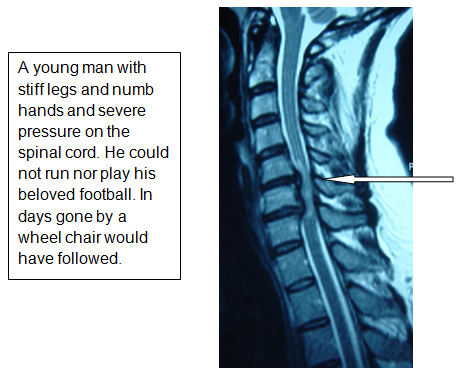
Gradually, the back of the disc and any osteophytes are cleared and the central canal is exposed thus gradually relieving the pressure on the spinal cord. This surgical part of the procedure is termed central canal decompression and the operation has slowed to a snail’s pace at this point as the spinal cord is immediately below. A specifically designed high speed air drill is used in this instance.
The nerves exiting the spine on either side are now cleared of any disc prolapse or osteophytes. This element of the operation is termed nerve root decompression. The removal of the disc prolapse itself is termed a discectomy.
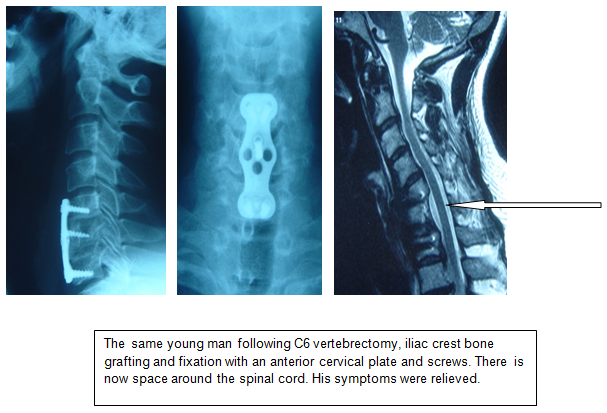
For patients that need a whole bone or bones and their associated discs removed so as to relieve pressure on the spinal cord and nerve roots over several levels, the operation is called a vertebrectomy/corpectomy.
Following a vertebrectomy/corpectomy, a fusion is always required.
We often need to harvest bone graft from the pelvic bone. This is done through a separate incision over the bony prominence of the pelvis near the front – usually on the right. A plate and cage are used to hold the spinal bones and any graft in place. This part of the procedure is called the reconstruction.
Next comes the final stage of the operation, called closure. Meticulous care is taken to stop any bleeding and the wound is then stitched in layers using internal absorbable stitches. A drain is often placed at the base of the wound. This is rather like a drip and is removed at around 24 hours. The skin is closed with a single stitch made of nylon. A dressing is applied. You will then usually need a collar fitted.
The suture is removed 5 days later by simply pulling on one end – do get an adult to help you!
Informed consent
Before you have a procedure of any kind, however trivial you may feel it to be, you must be fully aware of the possible and likely consequences. You have to sign a consent form in which you state that you are fully aware. We will go over this with you in your consultation. Do not sign the consent form for a procedure with us unless you feel fully informed of its aims and risks, as well as the alternatives.
Please make sure you are fully content with everything set out in our Informed Consent for Treatments: Operations and Injections.
What alternative procedures are there?
Much of this will have been discussed in our consultations. Essentially, an operation is always the last resort. Instead, you could try injections or further conservative treatment (physiotherapy, osteopathy, chiropractic, acupuncture, tablets and time). Obviously, we will usually have formed the view that these are unlikely to bring you to comfort any time soon before recommending surgery. For the majority, it is pain that drives the surgery. In these circumstances, you have to feel that the degree of pain warrants the risk and effort involved in putting yourself through the operation.
What are the Risks?
No procedure is without risk, though these are routine operations which rarely cause harm. If you would like to read an extended list regarding the risks of this particular type of surgery. Please click here for a extended information.
No procedure is without risk, though these are routine operations which rarely cause harm.
Chest infection and blood clots in the deep veins of the legs – these complications can result after any operation and indeed after any long period spent in bed. We can reduce the incidence of these by giving you injections to thin the blood, supportive stockings and compression pumps on the legs worn while in bed.
Risk to life and limb – Any anaesthetic and any operation may kill you. Any spinal surgery may paralyse you which in the instance of a cervical operation could mean loss of all arm, leg, bowel, bladder and sexual function. These disasters are extraordinarily rare. People do get run over by buses but it is exceptionally rare.
Swallowing – Problems with swallowing such that food feels difficult to get down or blocks can arise temporarily after the surgery but seldom persists for more than a few days. Likewise, the hoarseness of voice.
Nerve root injury – the nerve root is often handled during the procedure and microsurgical technique is used to reduce any damage. However, the risk of an individual nerve being permanently lost is around 1%.
Failure of an operation to achieve its intended goal is always possible. It is not uncommon for a degree of pre-existing weakness and numbness to persist.
The longer they have been present, the more likely this is. However, most patients experience an improvement, if not a complete resolution of their symptoms.
Recurrence of symptoms may occur. Post-operative physiotherapy plays an important role here. Scarring around nerve roots that are hypersensitive from previous surgery or a recurrence of the original disc prolapse can occur.
Operations simply tackle current troubles and offer no protection against future problems but post-operative physiotherapy can.
Deterioration – this is a possibility. Operations can make you worse, can do you harm or may leave you with new problems to cope with. This is rare and affects fewer than 1% of patients.
Wound infection can occur with any operation. In the spine, this is rare as there is so much muscle covering it. Muscle fights infection well. However, if an infection does set in, the effects can be very serious.
When can I go home?
Most people go home on or around the third post-operative day.
Post-operative neck care
Before you go home after your operation, we will have discussed some details of how to care for your neck in the weeks that follow. Please click here for a general summary.
Physiotherapy
If you develop pain on doing your specific instructed exercises, you should stop them. In the first few weeks, all that can occur is the simple healing process. Physiotherapy maintains your mobility during this time but should not be allowed to interfere with the healing process. Therefore, if it hurts you should stop. Physiotherapy begins in earnest around the fourth week when the wound and neck will be stable enough to allow real progress to be made.
Exercise
The aim here is to do small amounts but often. Problems arise when patients do a little too much a little too often. For most of the first week, you will either be in hospital or should be pottering about inside your home. For the second week, the amount of activity undertaken should essentially be unchanged. You should not be doing housework or looking after others. You may go out for short walks. From the second week onwards, light exercise may be undertaken. You may go on very short car journeys (10-15 minutes) and go out for longer walks. Prolonged outings and lengthy trips to the office will be bad for you.
Sitting
You are better to sit upright and not to have the neck bent by cushions. When lying on your back in bed, do not use too many pillows. Be careful about time spent sitting at a computer as this tends to stiffen the neck.
Baths and showers
You should in the early days avoid baths as any waterproof dressing is unlikely to keep out all water if submerged. Showers or and assisted standing baths are better. Please do not fall over.
Sex
If it hurts, don’t. If you think it will hurt, don’t – until of course you think it won’t and it doesn’t.
Wound care
You should not get the wound wet until the day after the sutures have been removed. It is perfectly reasonable to have a shower, providing the wound is covered with a waterproof dressing. The ward may provide you with this before you leave. It is best to cover the wound in a waterproof dressing for showers but this should be replaced by a dressing which breathes – ask our spinal nurse which ones you need.
Removal of stitches
The stitches, of which ever type, should be removed at or shortly after the fifth day from the neck but not until the tenth day from the hip. Most often a nurse linked to your GP or the district nursing service do this. You need to have agreed an arrangement for this to be done before you leave hospital – our ward nurses will liaise with your GP, district nurse or your local hospital as appropriate. You will also be given a ‘clip remover’ for you to give the nurse who will be doing the removal.
Bending, lifting, carrying
In the first few weeks, you should not be doing this. The physiotherapy, which will usually begin about the fourth to sixth week, will teach you how to bend correctly and how best to lift. It should certainly be something that you keep to a minimum in the first months.
Driving
In the first few weeks, you should be driven i.e. you should not drive the car yourself. In the weeks that follow, you should limit journeys to short periods. In general, it is best to have the car seat set as high and as upright as possible. Unless you can look over your shoulder, you are not considered safe to drive. If in doubt, do not drive until we give the all clear.
Sports
You should not do this until we have reviewed your progress. If should be deferred until you have completed the fitness programme that only begins with the physiotherapy at the fourth to sixth week and is likely to take a further four to six weeks at least.
Our general philosophy
The aim is for you to avoid things which aggravate your pain. Once recurrence of neck and arm pain has occurred, it is much more difficult to go away. It is much simpler to avoid it in the first place. It is not so much what you do but how often you do it.
*If you feel you are developing unexpected troublesome or worrying symptoms, do not hesitate to call The Spine Surgery London or the ward staff, who will be able to guide you.
When is my first follow up after surgery?
Our usual routine is to see patients three to four weeks after discharge and it is at this point that we can start the physiotherapy. Often there is a need for follow-up X-rays so it is useful to have the old ones for comparison, so please bring these with you. I usually then see you after another six weeks and then after a further three months.
When can I go back to work?
This may reasonably be anytime between four and twelve weeks post surgery. Please click here for a extended information.
This may reasonably be anytime between four and twelve weeks post surgery.
This might seem like a ridiculously wide window and certainly we will advise you more precisely. In fact, some patients are back at work inside two weeks and others still off at four months. Whatever the work, a gradual return is best. Days spent working from home may help. However, done in a graduated way, the return to work is a very positive part of your rehabilitation. It needs to be in your control and with the encouragement of your employer. If they can put up with you being part-time and unreliable, they will see you sooner. Discuss the advice we give you and make a plan with your employer.
What do I do in the event of problems?
If, once you get home problems arise, help is available from a number of sources. Firstly, if it is during working hours, you may ring The Spine Surgery London. If it is out of hours, our voicemail will tell you what to do in the event of an emergency. Secondly, you may ring the hospital and ask to speak to our Spinal Nurse Specialist. In her absence, you should ask to speak to the hospital’s Duty Manager or to the ward staff (please go to Contact Us page for suitable contact numbers).
You may of course contact your general practitioner or any emergency service, should you so wish or if the other avenues fail.
We do not provide a 24 hour emergency service but can respond on most occasions.