These procedures are performed via a keyhole opening. The primary aim is to relieve leg pain/sciatica caused by pressure on the nerve roots. (These operations are not designed to relieve back pain.)
Most commonly the problem is caused by a degenerative and prolapsed disc, pressing on the nerve root just prior to it emerging from the lumbar spine. The removal of the disc prolapse (not the whole disc but the ‘pea’ which has broken free from it) is what is referred to as ‘discectomy’ and when performed through a keyhole as in this instance, it is termed ‘microdiscectomy’.
“Decompression” just means removing any obstacle such as osteophytes, thickened ligaments in addition to any disc prolapse that is compressing the nerve roots. The widening thereby of the nerve’s exit hole, (nerve root foramen), is what is meant by ‘nerve root decompression’ or foraminotomy.
If the central spinal canal has been narrowed and all the nerves passing that point are compressed it too will be widened and this is called a “central canal decompression”.
You may in this type of surgery need one, two or all three of these procedures – i.e., microdiscectomy, nerve root decompression and central canal decompression. All this gets done at the same time through the same opening.
How is the operation done?
The surgery is carried out through the small opening in your back from which a tunnel is made through the tissues about a fingers depth into the spine where the nerves are under pressure. Guided by X-ray and with the vision of an operating microscope, the pressure is gradually relieved until all the nerves are released and any disc prolapse cleared.
Please click here for details of how the operation is performed.
Keyhole lumbar microdiscectomy, nerve root and central canal decompression
Once you are anaesthetised, you are taken through into the operating theatre and placed face down on the operating table. A slight curve is placed in the operating table so as to open the spine. We use an Image Intensifier, (X-ray machine), to determine precisely where we will need to make the incision, (cut in the skin).
Before the incision is made, local anaesthetic is also used to numb the area of skin and the muscles below. This reduces the amount of painkiller the anaesthetist has to use with the general anaesthetic and makes it safer. Also, the local anaesthetic has adrenaline in it so as to constrict the local blood vessels. This decreases bleeding which makes the operation safer and lengthens the effect of the local so as to lessen the immediate post-operative pain. This is called a ‘local block’.
A vertical cut in the centre of the lumbar spine, is then made which is usually in the region of 1.5 – 2 cm in length. The muscle is parted to reveal the bone over the back of the spine. An internal opening into the spinal canal itself is made called a “fenestration” and it is through this that we see with the operating microscope.
If the spinal canal is narrowed (central canal stenosis) or if the disc fragment is too big to remove without first widening the spinal canal, we first perform a central canal/spinal canal decompression. We then remove the disc prolapse and any pulp lying within the disc that seems likely to herniate at a later date – this is the microdiscectomy. The foramina (hole) which the nerve root exits from the spine is widened as necessary by shaving bone and ligament from the walls which have thickened to cause the narrowing – this is the nerve root decompression. When there is no more pressure on the nerves, the job is nearly done.
Any bleeding is controlled and if there has been leakage of spinal fluid this too is controlled. Then the wound is ready for closure. We do this mainly with absorbable internal stitches. A drain is sometimes placed at the base of the wound - this is rather like a drip and is removed after 24 hours. This skin may be closed in a number of ways though most commonly a single stitch made of nylon will be passed under the skin from one end to the other. Removal of the suture occurs at approximately 10 days by simply pulling on one end. This can be done either at the hospital or at your GP’s surgery or at home by the district nurse.
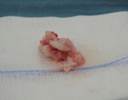
A prolapsed lumbar disc following removal
What if you have had surgery before?
This is referred to as revision surgery and whilst it is still routine and safe there are certainly some challenging elements to it.
Please click here for details.
First there is the scar on the skin. We attempt where possible to use the old scar. Often, because of our keyhole techniques, not all of the original scar needs to be opened. Sometimes it is not correctly positioned for us and a fresh incision is needed.
Next are the scars that will have formed between the muscle and the bone. These have to be dissected through. Often, this is quite traumatic and some bleeding will occur though occasionally it is actually quite straight forwards.
The most taxing problem lies in the spinal canal where scarring will have led to the nerves, bone, discs and any osteophytes all being encased in one solid mass. We begin by finding the nerves above and below the scar and then millimetre by millimetre we trace them in to the centre until we meet ourselves coming the other way. This takes a good deal of time and painstaking work.
There is clearly and enhanced risk of CSF leakage – probably in the order of 1 in 10 cases.
In addition, because the tissues have been traumatised twice and the operation takes longer and hence the wound is open for longer, there is an enhanced infection rate though this is still small.
We are often referred work with patients needing revision surgery and the trick is to go slowly. Whilst increased operating times do enhance some risks, nerve injury is the unacceptable alternative.
Likewise, because the nerves get more handling there can be some numbness and weakness after the surgery, particularly if this was a feature pre-operatively. It will nearly always recover quite quickly.
You might think that once a lesion had recurred once it couldn’t happen again. Sorry, not true. Think of it like the lottery – you are incredibly unlikely to win once, but, having won once you are no less likely to win a second time than the next man is to win for the first time. In fact, revision surgery has a higher failure rate than first time surgery.
What happens after the surgery?
Normally, you mobilise from the bed a few hours after the surgery and go home at around day three or four. However, rather than having a fixed idea about when you are going home we suggest you are ready. This will vary from person to person. The time of your discharge is something we will discuss with you in the days that follow the surgery.
Click here for extended information regarding the post operative period.
The post operative period
There will usually be an intravenous drip in one of the veins in your arm. This gives you fluids so you do not need to eat or drink if you feel sick. The anaesthetist may wish for you not to eat or drink for a while after the operation and will advise you of this. Most of you are soon having a cup of tea.
In addition, there will often be a separate small drip providing you with pain relief. Usually, there will be a button for you to press in order for the pain relief to be delivered i.e., you will control the amount of pain relief you get. This is a very safe and effective way of making sure you get analgesia when you need it. You cannot overdose yourself by pressing it too much – the device will simply fire blanks when the maximum safe dose has been reached. Often, you only really get pain when you move. It takes a little time for the pain relief to work. A good tip is to press the button a few minutes before you want to move. Some patients find that too much causes a headache or nausea. If this is a significant problem, we will need to use a different system but for most people it is the most effective way to deliver pain relief.
There will sometimes be a drain coming from the wound. This is like a drip and will be connected to some sort of collection device (small plastic bottle) next to you. This is usually removed the next day.
Wound care is important. You will have some form of surgical dressing on the wound – usually a light waterproof but “breathing” dressing. The wound should not be allowed to get wet until the day after the suture is removed. In general, we like to disturb the dressing as little as possible. If it becomes stained but is intact, it is often better to put one over the top rather than to take it off.
If you need to go to the toilet you may normally get up and use the facilities in your bathroom. If you are on bed rest (see paragraph below) or are in too much pain to do that then ask for a bottle or bed pan.
Nearly always you can get up immediately if you wish. Of course, you should have a nurse or physiotherapist with you on the first occasion.
CSF Leaks
About one in twenty times, there will be a leakage of fluid from the sack containing the nerves and this needs to heal before you get up. The fluid, cerebrospinal fluid, or CSF, is clear and watery. We can see the leak at the operation and will tell you of the event. Whilst this does not adversely affect the outcome of the operation it does mean you have to lie flat for five days. You may not get up at all for any reason. This is a great bore though as mentioned does not alter the outcome of the operation. During this time you can role over or lie on your front if you wish but you must not end up with your head higher than your bottom. The column of fluid in the spine extends up to the head and thus if the head is high compared to the base of the spine, fluid will tend to escape into the wound.
What Are The Risks?
No procedure is without risk though this is a routine operation which rarely causes harm and usually works very well.
It is vital that you are aware of the risks before you consent to surgery. We expect you to have read the information we provide if you are having surgery with The Spine Surgery London.
Click here for details of the risks associated with surgery and this operation in particular.
The risks of keyhole lumbar spinal surgery
Complications of any operation and indeed any long period spent in bed include chest infection and blood clots forming in the deep veins of the legs (deep venous thrombosis or DVT). Parts of the blood clots may break off and fly up to the lung where they block the blood flow (Pulmonary embolus or PE). Very rarely people die from these blockages. You may have heard of these complicating long plane journeys. We can reduce the incidence of these by giving you injections to thin the blood, supportive stockings (which I request you wear at all times whilst in hospital) and compression pumps on the legs worn while in bed. We use the stockings and pumps in theatre but do not start the injections until 24 hours after the surgery so as not to provoke bleeding into the fresh wound.
There is a risk to life and limb. Any anaesthetic and any operation may kill you. Any spinal surgery may paralyse you which in the instance of a lumbar operation will mean loss of all leg, bowel, bladder and sexual function. At its worst, this may be complete and permanent. Such disasters are extremely rare and are in the order of the risk of you being run over by a bus. People do get run over by buses but it is exceptionally rare. Of course, if you do not have the operation the disc may fully prolapse and paralyse you itself. Again, we see this though it is very rarely. In other words, there are buses on which ever road you choose, they occur in approximately equal numbers on the two routes and rationally they should not influence your decision – though they clearly often do. These buses are indeed extraordinarily rare and you can usually see them coming and so take evasive action.
The “cauda equina syndrome” is the term used to describe paralysis of this part of your nervous system – the spinal nerve in the lumbar canal. The patient usually has a phase of excruciating pain followed by numbness, paralysis and an inability to pass urine which classically is painless. i.e., you know you have an overfull bladder but it does not hurt – “painless retention”. An early warning may be numbness around the perineum/private parts/the area where your pants go. If you notice anything like this you need to see a doctor, any doctor – don’t wait for us - immediately. This syndrome is a surgical emergency. You need to have the disc removed immediately i.e., that day / night.
Nerve root injury affecting just the nerve that is being pressed on by the disc prolapse is not quite so rare but is far from common. Obviously the nerve root is handled during the procedure and even though microsurgical techniques reduce this to a minimum the risk of an individual nerve being permanently lost remains. It is low – less than 1 %. This might mean that the ability to stand on tip toe is lost or to lift up the foot (a foot drop) results. Again, if you do not have the operation pressure from the disc prolapse may do this anyway.
The spinal nerves are contained in a sack and this is filled with fluid secreted by and in communication with the brain. As the disc fragment presses directly on this sack, it may leak cerebrospinal fluid during the course of the operation. This should not adversely affect the outcome of the operation though does mean you will need to lie flat for five days as described above. Nearly always the leak can be seen during the surgery and therefore I will give instructions for you not to be mobilised for the five days. If you are told you may get up then I have not encountered a leak. This occurs about 1 in 20 times though is more frequent when patients have had surgery before.
Failure of an operation to achieve its intended goal is always possible. In this instance, it will mean the persistence of leg pain as it was before. This is uncommon though remember the purpose of these particular operations is to relieve leg and not back pain. The latter may remain though is often reduced to some degree. Further, rehabilitation for the back pain is more likely to prove effective when the nerves are no longer compressed and the legs are free. That is to say we get rid of the leg pain with surgery and the low back pain thereafter with rehabilitation physiotherapy. The persistence of some non-disabling levels of back pain is common after disc prolapse. For some years, fusion was added to the operation in an attempt to reduce the numbers of patients left with back pain. However, this involves a major opening of the spine, the insertion of large screws and rods along with bone grafting. The outcome was worse than with microdiscectomy alone and now fusion is no longer done in this context. It is not uncommon for a degree of pre-existing weakness and numbness to persist particularly if it was severe beforehand. The longer they have been present the more likely this is. However, most patients experience an improvement in weakness and numbness if not complete resolution.
Recurrence of symptoms may occur. That is to say you may get better only for things to get worse again later. There are a number of reasons why and again this may be in the form of back or leg pain. Back pain may occur in acute bouts and can be minimised by your being diligent with the post-operative physiotherapy. Leg pain may arise from a disc prolapse occurring at an adjacent level, a recurrence of the original disc prolapse, scarring occurring around the nerve root affected by the original disc prolapse, or damage caused by the original prolapse leaving the nerve root hypersensitive as it attempts to recover in the post-operative months. Usually, it is an element of each of these pathologies which operate together to cause recurrent leg pain. A degree of pain is not uncommon at times in the early phase though will usually settle over a period of a few weeks or months. Seldom are the troubles serious and rarely do they then persist though precisely how often is still a matter for some debate. To find out a true recurrence rate, thousands of patients need to be followed for tens of years and for none drop out during that time. There has been no perfect study but it is our impression from those studies that have been done and from our experience that perhaps 1 in 10 patients at some point in the future get into substantial recurrent trouble. This of course largely reflects the natural history of disc disease rather than anything relating to the surgery itself though it is important that you appreciate the operations simply tackle current troubles and offer no protection against future problems at other levels – the post-operative physiotherapy perhaps does. Obviously, we would not offer the surgery if we did not think that without it you are likely to fair worse than you are with it.
Deterioration is a possibility. Operations can make you worse, can do you harm or may leave you with new problems to cope with. This is rare and deterioration, directly as a result of the surgery, probably affects a fraction of 1% of patients. Quite a few patients may have a transient increase in numbness or weakness though persistent significant problems are rare indeed.
Wound infection can occur with any operation. In the spine, it is rare as there is so much muscle covering it. Muscle fights infection well. However, if an infection ever sets in the effects can be very serious. Again the risks are less than 1%. Diabetic patients are at slightly higher risk of this.
Informed consent
Before you have a procedure of any kind, however trivial you may feel it to be, you must be fully aware of the possible and likely consequences. You have to sign a consent form in which you state that you are fully aware. We will go over this with you in your consultation. Do not sign the consent form for a procedure with us unless you feel fully informed of its aims and risks, as well as the alternatives. Please make sure you are fully content with everything set out in our Informed Consent for Treatments: Operations and Injections.
Click here for details of for an extract
Obviously you must know what the aims and risks of any operation are. We will document in the notes that we have explained these to you as it is routine to do so. Do not sign the consent form if you feel we have not.
We will write something like this in your notes:- make sure you feel it is true
“I have explained the aims and risks of the procedure including those to life and limb (ie. death paralysis and disaster), of failure (the procedure does not work), recurrence (you get better but it comes back) and deterioration, (you are made worse), of death, paralysis, wound problems, of nerve/ nerve root injury, as well as the likely natural history of the condition (what happens if nothing is done), the possible impact of alternative managements and treatments, along with the usual post procedure recovery and its variants (i.e., how much time off from work, what help you will need at home, what the wound care is).”
These are all things you will need to have had covered. Again, do not sign the consent if you are not sure
What happens if you don’t have it done?
The “natural history” is what happens when nothing is done and this must be compared with the scale of risks associated with the procedure.
Click here for more details
Eventually many people’s troubles will settle though again good data is hard to find. A general rule of thumb is that within the first six to ten weeks spontaneous resolution occurs for about 95% of patients – or at least a substantial and consistent decline in symptoms is evident. If you are having surgery before this time there needs to be a good reason – progressive motor or sensory loss, worsening rather than consistent or declining pain or a disc prolapse of such immense proportion that it threatens paralysis. You should know what the reason is for such rapid progress. However, if after this time there is no clear pattern of decline in symptoms many of you are stuck at least for a long time. Into this picture it may be reasonable to integrate any social, personal, occupational and domestic pressures.
What are the alternatives?
Please click here for details.
Much of this is covered elsewhere and will form part of our discussions. Endoscopic spinal surgery is the principle operative alternative. If this is relevant to you we will discuss it. However, any operation is always the last resort. Instead you could try injections or further conservative treatment (physiotherapy, osteopathy, chiropractic, acupuncture, tablets and time.) Obviously, we will usually have formed the view that these are unlikely to bring you to comfort any time soon before recommending surgery. Occasionally, we will have warned you that bad paralysis of nerves may occur if things are left and in these circumstances there is little choice but to proceed though this is rare. For the majority, it is pain that drives the surgery. In these circumstances, you have to feel that the degree of pain warrants the risk and effort involved in having the operation.
Discharge
Most people go home on or around the third post-operative day. However, there is no rush and you should stay until you are ready.
Please click here for details of how to time your discharge
Planning your discharge
Do not have a fixed plan. Make arrangements that are flexible. Surgery is not like fixing a new car.
You need to be recovered enough so that you can manage the journey home, life at home and have not needed the pain relief drip for 24 hours. If you live a long way off, are on your own or have a dependant young family you will need to stay for longer. Occasionally, the less able who live alone might sensibly use a convalescent facility. Equally, some go home on day one or two though if you are an early leaver you should rest at home as if you were still in hospital.
Remember there is no rush - go home when you are ready. You should be able to tick certain boxes:
- be able to mobilise and more or less dress yourself
- to have passed urine and opened your bowels
- to have tried some stairs with the physiotherapist
- to be able to manage on just oral medication and pain relief.
- to be able to cope with your journey home
- to be able to survive comfortably with your personal home circumstance
Often day two and three are worse than day one in terms of pain. We tend to plan the precise discharge time on the ward round on day two or three.
How to get home
The front passenger seat in a standard car is fine. If the journey is long get out of the car every hour and do some simple stretches. Then get back in and carry on. It is often sensible to take some tablets before you leave the ward. Go to bed when you get home regardless of how you feel.
Done once, even a long journey is OK. This is not a licence to drive every day – see below.
Post-operative back care
This is obviously crucial to any procedure’s success. Even before you come in and again before you go home after surgery, we will have discussed some details of how to care for your back in the weeks that follow. Indeed several members of the team will be involved in this. Below we give a general summary.
If you feel you are developing unexpected, troublesome or worrying symptoms, do not hesitate to call our office or the ward staff. If troubles arise out of hours call the hospital and ask for the sister in charge.
Please click here for details of post operative back care.
Post-operative Back Care
Physiotherapy
You may well have been given specific instructions by the hospital’s physiotherapist. Indeed you are likely to be given a sheet with diagrams of various exercises. The precise details of these exercises and how often they should be done are of less importance than your response to them. That is to say, if you develop pain on doing these exercises, you should stop them. In the first few weeks all that can occur is the simple healing process. Physiotherapy maintains your mobility during this time but should not be allowed to interfere with the healing process. Therefore, if it hurts, you should stop and you should not be anxious if, as a result, you are quite stiff by the end of this early period. Physiotherapy begins in earnest around the fourth week when the back will be stable enough to allow real progress to be made.
Exercise
The aim here is to do small amounts but often. For most of the first week you will either be in hospital or should be pottering about inside your home. For the second week the amount of activity undertaken should essentially be unchanged. You should simply be moving about as if you were in fact still in hospital. It would be perfectly reasonable to fix your own meals and to look after yourself though you should not be doing housework or looking after others. You may go out for short walks. From the second week onwards, light exercise may be taken. You may go on very short car journeys (10-15 minutes) and go out for longer walks. Prolonged outings, lengthy or frequent trips to the office will be bad for you. Problems most often arise when patients do a little too much a little too often, i.e., one trip to the office may be alright but three cause troubles.
Sitting
You are better to be standing or lying following back surgery. If you wish to sit, a high, upright dining room style chair is the most appropriate. It is certainly reasonable to start sitting for your meals when you have gone home but it is sensible to stand up and stretch between courses. This should be back to normal around about the four to six week mark. However, it will always be advisable to avoid prolonged periods sitting and very soft or low armchairs.
Sex
If it hurts, don’t. If you think it will hurt, don’t - until of course you think it won’t and it doesn’t.
Wound care
You should not get the wound wet until the day after the sutures have been removed. It is perfectly reasonable to have a shower, providing the wound is covered with a waterproof dressing. The ward may provide you with this before you leave. In general, we like to change the dressings on wounds as infrequently as possible. The wound should be kept dry and a dressing used that allows the wound to breathe.
Removal of Stitches
The stitches should be removed at or shortly after the tenth day. We mostly use a single stitch which runs under the skin and can be pulled from one end. (Get an adult to help you.) I also usually put steristrips (small sticky tapes) across the wound and two in parallel with the wound to hold the stitch ends. The ones holding the stitch ends need to be pulled off and then the suture can be removed. Most often a nurse linked to your G.P. or the district nursing service do this. If you are near one of my hospitals you may be able to have these removed there. You need have agreed an arrangement for this to be done before you, leave hospital - our ward nurses who will liaise with your GP, district nurse or one of the local hospitals as is appropriate.
Bending, lifting, carrying
In the first few weeks you should not be doing this. The physiotherapy, which will begin about the fourth to sixth week, will teach you how to bend correctly and how best to lift. It should certainly be something that you keep to a minimum in the first months.
Driving
In the first few weeks you should be driven i.e., you should not drive the car yourself. In the weeks that follow, you should limit journeys to short periods. As physiotherapy commences and progress is made, you may gradually start to extend this. In general it is best to have the car seat set as high and as upright as possible. If you are becoming uncomfortable you should stop, get out and do some light stretches before continuing.
Sports
You should not do this until we have reviewed your progress. It should be deferred until you have completed the fitness programme that only begins with the physiotherapy at the fourth to sixth week and is likely to take a further four to six weeks at least.
General philosophy
The aim is for you to avoid things which aggravate your pain. Once recurrence of back and leg pain has occurred, it is much more difficult to get it to go away. It is much simpler to avoid it in the first place. If in doubt, err on the side of caution. You can do most things after the first week or so. However, you will not be able to do much of them. “Can I drive?”, “pick up the baby?”, “go into the Office?” or “fly?” are all frequently asked questions. The answer is usually yes BUT not very often. It is not so much what you do but how often you do it.
Follow-up
The usual routine is to see patients three or four weeks after discharge and it is at that point that we can start the physiotherapy. This will need to be near to home though later may need to move nearer to work. We usually then see you after another six weeks and then a further three months.
Return to work
Click here for details
Planning your return to work
This may reasonably be anytime between four and twelve weeks post surgery. This might seem like a ridiculously wide window and certainly we will advise you more precisely. In fact, some patients are back at work inside two weeks and others still off at four months. A brick layer commuting 50 miles by car each way will take longer than a librarian working next door to home.
Whatever the work a gradual return is best – perhaps two half days the first week (Tuesday and Thursday), three the second (Monday Wednesday and Friday) and four the fourth (Monday, Tuesday and Thursday, Friday). Work five half days the next and then start to increase the length of the days. It is important to keep up the physiotherapy during this phase. The program outlined above is very gradual and more rapid progress may be possible but if pain recurs you should ease off.
Done in a graduated way, the return to work is a very positive part of your rehabilitation. It needs to be in your control and with the encouragement of your employer. If they will put up with you being part-time and unreliable they will see you sooner.
If, by contrast, your job is one whereby you have to be there fulltime and reliably or not at all, it will take longer. Then the job is not a part of the rehabilitation but the hurdle rehabilitation has to prepare you for. You will get back later as you need to fully recovered before starting. If you have a long commute your return will be further delayed. The average commute time for my patients is in the region of one hour each way. From the spinal perspective, that is a two hour physical job in addition to your real work. Days spent working from home help.
Discuss this advice with your employer and make a plan. Obviously, the best laid plans may change due to circumstances and I will advise on how likely your plan is to come off at the first out-patient session post surgery i.e., at about the four week mark.
Return to sport
Please click here for details of how to return safely to sport.
A safe return to sport
Clearly, the situation is different for the occasional exerciser than it is for the keen amateur sports person. Equally, the elite athlete or professional sports person will have particular demands. Certain sports are more trouble than others. With that in mind, here is some general advice tailored to the two broad groups:-
Advice for the amateur
In general terms for members of the general public, it takes three months to get over the surgery and return to normal life. It takes a further three months to train you back up to competitive sport.
Some sports are tougher than others. We would not recommend significant long distance running, rowing machines or squash, (tennis and badminton are usually fine). However, most other sports are fine- after an appropriate training schedule to get you fit and to strengthen the spine.
Two sports need a special mention. You should miss a ski season, i.e., this needs to be a good six months off. Likewise, it should probably be six months before you do serious riding – much depends on the horse of course! Essentially, done properly, skiing and horse riding are like advanced Pilates or core muscle exercises, i.e., they can be good for you. However, you would not leap into an advanced Pilates class any more than you would yoga and neither would you expect to do them if you were injured.
You may get back to your sport safely when the disc has firmly healed, (and you can do nothing to speed that up), and when you are cardiovascularly fit have achieved good flexibility and basic core muscle strength. Your physiotherapist will guide you.
It is all about being reasonable and phasing in the return. Start with a few holes of golf and don’t go for the big drive on your first few visits. Make sure there is time to recover before and after you play. Gently build it up.
Whatever your sport now is a good time to see a coach. Most professionals have injuries and there are ways to T off, to serve, to set up your bike and even to run, that are more back friendly than others. A professional coach will be able to help you if you explain your problem – “I have a bad back and want to run like Usain Bolt, please”. Good luck.
Elite or professional sports people
For elite athletes, the situation needs to be tailored to your specific sport and any neurological weaknesses. The latter can be frustratingly slow.
We can nearly always get you doing fitness work within a few weeks and will often use water-based exercise.
The younger you are, (i.e., the earlier in your career), and the tougher the sport is for the spine, the longer it takes. Likewise, many of you will have other injuries we need to work around.
There are nearly always specific competitions and events you are hoping to target and we will tailor the return to play in that context as much as is sensible.
We will always need to look at the routine of your training, as well as technique if we are to prevent further injury. This is where the cause of so many injuries hides. It is therefore a process that will involve not only your physiotherapy team, but the coaches and managers so that with you we can put together the strategy most likely to see rewards.
It is the routine that most of you get back to your professions.
The trick is to cover all the angles and the devil is in the detail. Do try to be patient. It is like trying to escape from a field full of lions – you have to plan the route exactly and if you bolt for it they will see you. Take it gently, very gently at first, until we are certain we are fit and fast enough to smile while we bolt over the horizon.
This philosophy has worked well for many.
Please click here for details of the teams and organisations we have helped.
The Results
The results of decompression or discectomy are usually very good and the postoperative course relatively quick. You should be back at work in a few weeks and it is the minority of you who will have substantial troubles afterwards. It is true also to say that most of you have some back aches after disc prolapse and when you have the arthritis which led to the surgery in the first place though only a small minority find this limiting or a burden. You can expect to get good relief of leg pain and for numbness and weakness to improve though this may take some time. There is an incidence of recurrence of both stenosis and disc herniation. Recurrent herniation is about 5% though it depends how hard you look, how long a period your follow up the patients and how severe a problem you register on any follow-up study. Stenosis, if you live long enough, will always come back though hopefully we will have sorted the problem out for a good many years.
What do you do in the event of problems?
If, once you have got home, problems arise, help is available from a number of sources.
Click here for details of who and how to call.
Where can I get help?
First, you may ring my office number. If it is during working hours this is certainly what you should do. My secretarial staff will be able to contact myself, my clinical assistants or our spinal nurse and obtain advice for you.
If it is out of hours you may also ring this number and the machine will tell you what to do in the event of an urgent enquiry or you may leave a message.
Second, you may ring the hospital and ask to speak to my Spinal Nurse. In her absence, you should ask to speak to the hospital’s Duty Manager or to the ward staff.
You may of course contact your general practitioner or any emergency service should you so wish or if the other avenues fail.
We do not provide a 24 hour emergency service but can respond on most occasions.
Costs, Codes and Authorisation
A separate information sheet is available which covers all aspects of this. Please obtain this and read it before you confirm your surgery. The costs of private surgery are considerable and if you are hoping to use insurance you will need to obtain authorisation from your insurer and register this with us prior to admission. Some insurers/policies may not pay all surgical, anaesthetic or hospital fees. All costs remain your responsibility even if your insurer has agreed to help/pay direct. There are usually three bills you need to know about; the hospital, the anaesthetist and the surgeon. You are responsible for ensuring all are paid.
Other sources of information
Please click here for details of other sources of information.
Other sources of information
We produce a number of other information sheets. You may obtain a title list from my office.
The Princess Grace Hospital produces information on a number of surgeries including spinal procedures.
We were also involved in their production so they are not entirely independent. However, the physiotherapy and nursing issues are given an airing. You can obtain these from our Spinal Nurse – see contact details below.
Your General Practitioner will have seen other patients going through this kind of procedure and they can offer valuable insights into the practicalities behind the surgery. Of course they may also be familiar with any other health concerns you have and be able to offer advice on how these might impact on recovery.